STORY AT-A-GLANCE
-
Following a downward trend from 2.1% in 2010 to 1.8% in 2016, severe obesity among children aged 2 to 4 years jumped back up to 2% in 2020
-
Among certain states and ethnic groups, rates were even higher; prevalence of severe obesity among 2- to 4-year-olds reached 2.8% in California as well as in Hispanic children
-
Severe early-onset obesity is linked with earlier and more severe chronic disease risk, including high blood pressure, dyslipidemia, prediabetes and early mortality
-
Duke University School of Medicine researchers described severe obesity in toddlers as a “canary in the coal mine for the health of future generations”
-
Top infant formulas are made largely of corn syrup and are associated with increased obesity risk in the first five years of life; breastfeeding is associated with a decreased risk of obesity
Severe obesity among children aged 2 to 4 years was on a downward trend, decreasing from 2.1% in 2010 to 1.8% in 2016. But research published in Pediatrics shows the trend is on the rise once again, with severe obesity reaching 2% among this toddler age group in 2020.1
Among certain states and ethnic groups, rates were even higher. Prevalence of severe obesity among 2- to 4-year-olds reached 2.8% in California as well as in Hispanic children. “We were doing well and now we see this upward trend,” study author Heidi Blanck of the U.S. Centers for Disease Control and Prevention, told the AP. “We are dismayed at seeing these findings.”2
Severe Obesity in Toddlers a ‘Canary in the Coal Mine’ for Future Generations
In the U.S., 1 in 5 children and adolescents is obese.3 Among 2- to 19-year-olds, the prevalence of obesity was 19.7% from 2017 to 2020, or 14.7 million individuals affected.4 Early obesity is strongly predictive of obesity in later life, with 90% of children who are obese at age 3 still obese in adolescence.5
Obesity in children raises the risk of many health conditions, including high blood pressure, Type 2 diabetes, asthma sleep apnea, joint problems and gallbladder disease. It also takes a mental toll and is associated with an increased risk of anxiety, depression, low self-esteem, social problems and lower quality of life.6
Severe obesity is particularly troubling, however, as severe early-onset obesity is linked with earlier and more severe chronic disease risk, including high blood pressure, dyslipidemia, prediabetes and early mortality.7 Even when compared with moderately obese children, those with severe obesity are at a greater risk of health problems such as:8
-
Cardiovascular disease
-
Metabolic syndrome
-
Type 2 diabetes
-
Fatty liver disease
-
Premature death
In a commentary, Duke University School of Medicine researchers described severe obesity in toddlers as a “canary in the coal mine for the health of future generations”:9
“Severe obesity is different than milder forms of overweight and obesity … Thus, these new data … showing reversal of previous progress, with an increase in severe obesity in children aged 2 to 4 years, is a cause for great concern for policymakers, clinicians, and public health professionals.”
NAFLD Is a Health Emergency in Children
Nonalcoholic fatty liver disease (NAFLD) affects 32.4% of people globally,10 and it’s the most common cause of liver transplant in adults under the age of 50.11 NAFLD also affects up to 9.6% of American children aged 2 to 19,12 making it as common as asthma.13 In 15- to 19-year-olds, prevalence is as high as 17.3%.14 As reported in a March 2021 paper on pediatric NAFLD, obesity is a driving force behind NAFLD in children:15
“The largest risk factor for NAFLD is obesity. Obesity and NAFLD in children are often associated; however, they are not concomitant.
In a 2019 study in 408 children with obesity using whole liver magnetic resonance imaging–proton density fat fraction, the prevalence rate of NAFLD was 26.0%, or roughly one in every four children. In the Teen LABS study of adolescents with obesity severe enough to warrant weight loss surgery, the prevalence rate of NAFLD was higher at 59%.”
The dramatic rise in NAFLD in early 2020 may in part be due to the COVID lockdowns, which had the effect of raising childhood obesity rates by 8.3% to 13.4%, depending on the age group.16 The Pediatrics study also cited the COVID-19 pandemic as having detrimental effects on children’s health:17
“Although our study did not capture data during the COVID-19 pandemic, it is important to acknowledge the substantial impact of the pandemic on the daily routines of children and adolescents. The pandemic has introduced various challenges, including reduced opportunities for physical activity, increased sedentary behaviors, limited access to healthy food, and heightened stress levels within households.
These factors can have significant implications for weight gain, particularly among children with excessive weight, and may potentially influence future trend in severe obesity.”
Why Are so Many Toddlers Severely Obese?
The study involved data from 16.6 million 2- to 4-year-old children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) from 2010 to 2020.
While the study authors suggested the increase is “likely influenced by a complex interplay of various factors,” citing levels of state social resources, funding to local WIC agencies and implementation of WIC benefits, such as breastfeeding support and nutrition counseling, separate research identified four factors that, when combined, account for 42.9% of childhood obesity by age 4.5 years.18 This includes:19
-
Lower food security during infancy
-
More than 1 hour per day of screen time at age 2
-
Sleeping 11.5 hours or less per night at age 2
-
Weekly to daily consumption of fast food and soda at age 2
According to the study authors:20
“Among children with no modifiable risk factors present, the prevalence of obesity was 4.4% vs. 20.7% when all four risk factors were present. Our findings highlight the importance of considering the impact of exposure to risk factors for obesity in early childhood not just in isolation but together and cumulatively.”
Among children in the WIC program, food insecurity (FI) could be a contributing factor. The Duke University researchers pointed out that although it seems paradoxical that decreased access to food would increase obesity, multiple studies confirm this association. “A proposed explanation is that FI leads to financial trade-offs, with basic needs (e.g., housing) forcing the purchase of cheaper foods that tend to be energy-dense but with low nutritional value.”21
That being said, U.S. data similarly suggests that 2.5% of preschool-aged children are severely obese,22 which includes those not affected by food insecurity. So, there are likely other key factors at play.
Corn Syrup Is the Main Ingredient in Many Infant Formulas
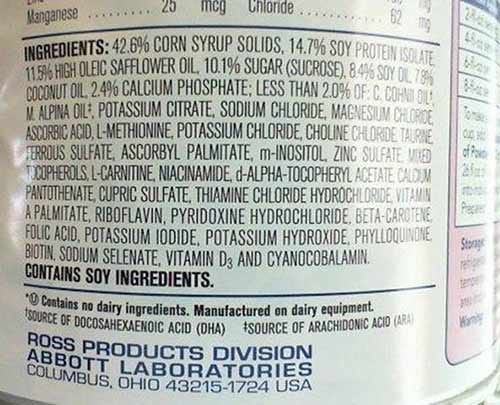
Despite the fact that breastmilk is the healthiest food for babies, only 62.6% of U.S. infants are exclusively breastfed immediately following birth.23 By 6 months of age, only 24.9% are exclusively breastfed. This means most babies are fed formula, which is a highly processed food product made largely of corn syrup, vegetable oils and sugar. You can see the ingredients for yourself on the label above, which is from one of the top recommended infant formulas in the U.S.
Not surprisingly, feeding infant formula may be driving obesity and other health risks in infants and toddlers. Research published in the American Journal of Clinical Nutrition found infant formula made with corn syrup solids is associated with increased obesity risk in the first five years of life, in a dose dependent manner.24 These sweetened formulas may also cause children to develop greater food fussiness, indirectly influencing obesity risk by shaping taste preferences early on.25
“While infant formula is designed to provide all the necessary nutrients for infant growth and development, it has been linked with infant hospitalizations and infections, childhood obesity, and lowered levels of docosahexaenoic acid (DHA), an important fatty acid related to brain development,” researchers wrote in npj Metabolic Health and Disease.26
Formula-fed infants are more likely to gain weight rapidly and in excess, a risk factor for childhood and adult overweight and obesity.27 Infants fed more infant formula than breast milk are also more likely to be overweight during older childhood and adolescence.28 Meanwhile, contaminants in formula may negatively influence neurodevelopment, even when they’re found at low levels.29
More Proof That Breast Is Best
Breastfeeding is associated with a lower risk of overweight and obesity. Children who are breastfed for more than one year are less likely to be overweight or obese between the ages of 6 and 16.30 Not only does exclusive breastfeeding prevent early introduction of foods that may trigger weight gain but it also establishes healthy gut microbiome, which is key for lifelong health. According to the Global Breastfeeding Collective:31
“Breastfeeding helps populate the child’s body with ‘good’ bacteria from his or her mother, which provide protection against excessive weight gain. Breastmilk contains hormones and other biological factors involved in the regulation of food intake that may help shape the long-term physiological processes responsible for maintaining energy balance.
Feeding of infant formula by bottle may interfere with a child’s recognition of satiety and thus lead to overeating.”
Further, the benefits continue into adulthood. One study found a 26% lower risk of becoming overweight or obese among adults who were breastfed.32 There are additional health benefits as well, including a lower risk of Type 2 diabetes, high blood pressure and cardiovascular disease as an adult.33 Breastfeeding also offers protection against allergies, enhanced immune system development and a boost for brain development.34
Even partially breastfed babies experience a beneficial change in their metabolome, or chemical makeup in the gut, that’s good for brain development35 and may translate to better test scores at age 2.36
Risky Surgery and Prescription Drugs Advised for Obese Children
Instead of tackling the drivers of childhood obesity, the American Academy of Pediatrics (AAP) gave a wholehearted endorsement for weight loss drugs and surgery in children as young as 12 and 13, respectively. “Waiting doesn’t work,” coauthor Dr. Ihuoma Eneli told the Associated Press. “What we see is a continuation of weight gain and the likelihood that they’ll have (obesity) in adulthood.”37
The AAP guidance recommends “comprehensive treatment,” which includes nutrition support, physical activity, behavioral therapy, medications and metabolic and bariatric surgery.
“There is no evidence to support either watchful waiting or unnecessary delay of appropriate treatment of children with obesity,” the guidance explains, instead setting the tone that early and aggressive drug and surgical treatment is warranted.38 Further, the guidelines specifically state:39
-
Pediatricians and other primary health care providers should offer adolescents 12 years and older with obesity (BMI ≥95th percentile) weight loss pharmacotherapy … as an adjunct to health behavior and lifestyle treatment
-
Pediatricians and other primary health care providers should offer referral for adolescents 13 years and older with severe obesity (BMI ≥120% of the 95th percentile for age and sex) for evaluation for metabolic and bariatric surgery
The AAP recommends the weight loss pill orlistat, Novo Nordisk’s semaglutide (Wegovy) — a diabetes drug given by injection — and the diabetes medicine metformin as potential obesity treatments in 12-year-olds and up.40 Each comes with its own set of risks. Orlistat can cause kidney and liver injury, along with gastrointestinal adverse effects, such as oily stools, diarrhea and abdominal pain, for instance.41
Wegovy, meanwhile, also caused gastrointestinal side effects, including nausea and vomiting, as well as concerns of pancreatitis, pancreatic cancer and retinopathy complications, including hemorrhage and blindness.42
Metformin’s side effects include a metabolic condition called lactic acidosis, which can be life-threatening.43 Subjecting children to surgery for weight loss is also egregious, as it can lead to permanent complications and even death.44 The AAP advice stops short of recommended drugs or surgery for preschoolers, as few of the studies they reviewed included children under 5. According to the Duke University researchers:45
“In the final recommendations, treatment options for children under aged <6 years include motivational interviewing (strong evidence) and intensive health behavior and lifestyle treatment (moderate evidence). None of the pharmacotherapy or surgical trials included in the CPG involved children <5 years; it is unclear whether these options will, or should, ever be used among preschoolers.”
Tips for Healthy Weight in Children
Part of the problem with the conventional model for treating childhood obesity is that children receive flawed nutritional guidance focused on reducing saturated fats and other whole foods, while promoting vegetable oils and heavily processed, low-fat diets.46
When you consume an abundance of ultraprocessed foods, it’s not only a matter of taking in “empty calories” or too many calories that cause weight gain. It triggers a catastrophic cascade of health declines rooted in mitochondrial dysfunction and insulin resistance.
Meanwhile, conventional nutritionists typically do not advise that increased intake of toxic industrially processed seed oils, often referred to as “vegetable oils,” are also driving obesity. Examples of seed oils high in omega-6 PUFAs include soybean, cottonseed, sunflower, rapeseed (canola), corn and safflower.47
Omega-6 is considered to be pro-inflammatory because of the most common variety, linoleic acid, which will radically increase oxidative free radicals and cause mitochondrial dysfunction.48
As researchers noted in the journal Nutrients, “In addition, a few studies suggested that omega-6 PUFA is related to chronic inflammatory diseases such as obesity, nonalcoholic fatty liver disease and cardiovascular disease.”49 Reducing your child’s intake of seed oils while increasing intake of healthy fats is a powerful way to support a healthy weight.
Engaging in nonexercise movement throughout the day, and getting regular exercise, will provide further benefits, as will avoiding obesogens in the environment, such as endocrine-disrupting chemicals found in contaminated foods and food packaging.50
Providing infants a healthy start via breastfeeding is also important, but if your child is obese, a holistic practitioner who understands the underlying drivers of obesity can provide a comprehensive strategy for weight loss that doesn’t involve drugs or surgery.
Source: Source link
Publish Date: