Originally published on: March 11th 2024
Originally published on www.jeffreydachmd.com
One of my patients underwent chemotherapy for lymphoma with a good result. The chemotherapy induced a complete remission. The para-aortic and mediastinal nodal masses melted away, and the follow up PET scan was completely clean, a complete remission. However only 3 months later, the lymphoma returned with a vengeance, even more aggressive than before. Over the next 3 years this was repeated three times. Each remission was followed by a relapse with more aggressive cancer behavior.
Pro-metastatic Effects of Chemotherapy
In 2020, Dr. Crescenzo D’Aletio reviewed the medical literature on this effect, writing chemotherapy has paradoxical pro-metastatic effects:
This review highlights the paradoxical pro-metastatic effects of chemotherapy linking reactive responses to treatment to tumor relapse and metastasis formation through primary tumor remodeling and generation of a favorable pro-metastatic niche.(1)
Dr. Crescenzo D’Aletio goes on to explain the mechanism of at play. The chemotherapy kills the “bulk” tumor cells, yet leaves behind chemo-resistant cancer stem cells, which repopulate with greater metastatic potential. The cancer stem cells repopulate under the intense stimulation of a massive systemic inflammatory response characterized by massive cytokine and chemokine release.
Breast Cancer Example
In the below quote, Dr. Crescenzo D’Aletio describes chemotherapy induced cytokine release which activates both the Wnt/β-catenin and NF-κB pathways creating an inflammatory feedback loop in breast cancer:
In breast cancer, cytokines released by tumor cells after chemotherapy can activate both Wnt/β-catenin and NF-κB pathways that amplify the secretion of further cytokines able to establish an autocrine inflammatory forward-feedback loop enriching for chemoresistant CSCs.(1)
Lung Cancer Example
A common chemotherapy drug for lung cancer is cisplatin, which kills bulk cancer cells, yet triggers massive IL-6 cytokine release which contributes to chemoresistance and prometastatic effects, resulting in increased distant metastatic disease formation. Dr. Crescenzo D’Aletio writes:
For instance, cisplatin treatment of lung cancer cell lines and xenografts triggers an increased release of the pro-inflammatory cytokine IL-6 [Interleukin-6] , that contributes to chemoresistance of cancer cells by activating EMT [epithelial to mesenchymal transition] and up-regulating anti-apoptotic proteins and DNA repair associated molecules [55]… Interestingly, despite primary tumor shrinkage, cisplatin-selection and priming of chemoresistant and metastatic CD133+CXCR4+ cells [Cancer Stem cells] results in increased distant metastasis formation.(1)
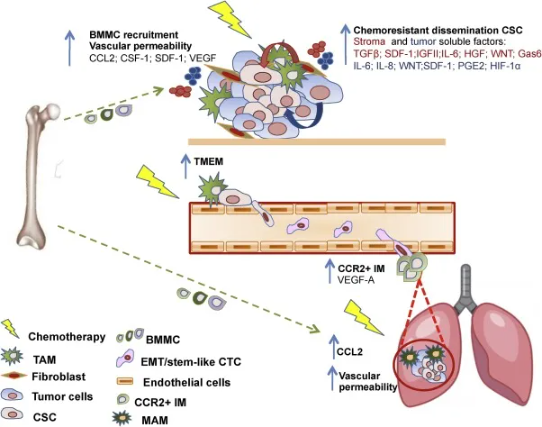
Above image : Fig. 2. Mechanisms mediating pro-metastatic effects of chemotherapy at different tumor districts. Courtesy of Dr. Crescenzo D’Aletio.(1)
Dr. Crescenzo D‘Aletio concludes that chemotherapy is overall unsatisfactory for control of metastatic cancer spread throughout the body, and actually induces this effect:
In several tumor types, chemotherapy has so far demonstrated an overall unsatisfactory potential to counteract and control metastatic dissemination even when a partial or complete response has been achieved at the primary tumor site [4]. This clinical issue could be in part related to host responses to chemotherapy activating reactive and reparatory mechanisms able to foster generation of CSCs [Cancer Stem Cells], primary tumor cells escape and distant site colonization [7] (Fig. 2). (1)
References
1. D’Alterio, Crescenzo, et al. “Paradoxical effects of chemotherapy on tumor relapse and metastasis promotion.” Seminars in cancer biology. Vol. 60. Academic Press, 2020.
At the primary tumor site, chemotherapy has been reported to promote selection of chemoresistant and disseminating tumor cells endowed with properties of cancer stem cells (CSCs) through activation of autocrine and paracrine self-renewing/survival pathways promoted jointly by therapy-selected tumor and stromal cells. Resistant CSCs represent seeds for tumor relapse and increased infiltration by immune cells, together with enhanced vascular permeability induced by chemotherapy, facilitates tumor cells intravasation, the first step of the metastatic cascade. As a consequence of primary tumor/metastasis re-shaping induced by chemotherapy, circulating tumor cells (CTCs) detected during therapy can display a shift towards a more mesenchymal and stem-like phenotype, conductive to increased ability to survive in the circulation and seed distant organs. At the metastatic site, host responses to therapy activate inflammatory pathways that ultimately facilitate tumor cells extravasation and metastatic colonization. Finally, cooperation of immune cells and endothelial cells at perivascular niches favors the extravasation of tumor cells endowed with high potential for metastasis initiation and protects them from chemotherapy.This review highlights the paradoxical pro-metastatic effects of chemotherapy linking reactive responses to treatment to tumor relapse and metastasis formation through primary tumor remodeling and generation of a favorable pro-metastatic niche.
Dr. Jeffrey Dach, MD, is the founder and Medical Director of a clinic in Davie, Florida specializing in bioidentical hormones, natural thyroid and natural medicine called TrueMedMD. To see his full Curriculum Vitae visit his website here.
© March 11th 2024 GreenMedInfo LLC. This work is reproduced and distributed with the permission of GreenMedInfo LLC. Want to learn more from GreenMedInfo? Sign up for the newsletter here https://www.greenmedinfo.com/greenmed/newsletter.
Source: Original Article
Originally published on: March 11th 2024


