Story at-a-glance
- Your skin microbiome helps protect against UV radiation damage by metabolizing harmful cis-urocanic acid (cis-UCA) using an enzyme called urocanase, preventing immunosuppression and inflammation after sun exposure
- Urocanase-positive bacteria rapidly respond to UVB exposure, shifting skin microbiome composition within hours and creating a protective feedback loop that supports overall skin health
- Conventional sunscreens often disrupt beneficial skin bacteria, while certain microbes produce protective compounds like pigments, antioxidants, and enzymes that naturally neutralize harmful UV radiation
- Linoleic acid (LA) from vegetable oils accumulates in skin cells, making them vulnerable to UV damage. Conversely, C15:0 fat can eventually replace LA in cell membranes
- Reducing LA intake and supplementing with 2 grams of C15:0 daily can help boost skin health in 12 to 18 months, enabling greater sun resilience without relying on conventional sunscreens
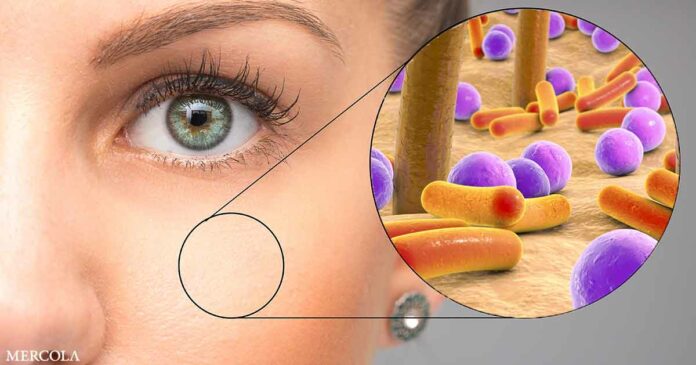
Aside from the microbiome living in your gut, did you know that your body is also home to other microbiomes, too? One example that doesn’t get enough time in the spotlight are those found on your skin.
Your skin forms a large, protective barrier against dirt, pathogens, and other substances that will affect your health. While your skin cells contribute to this defense, it also contains microbes actively protecting it from harmful solar radiation.
Your Skin’s Defense System Depends on Microbes
A study published in The Journal of Investigative Dermatology explored whether certain skin-resident bacteria producing a unique enzyme known as urocanase (UCA) could neutralize the harmful effects of cis-urocanic acid (cis-UCA), a chemical compound produced on your skin after ultraviolet-B (UVB) exposure.1 To create the context, the researchers noted:
“[C]ertain skin bacteria specifically metabolize cis-urocanic acid, a photoproduct of a major UV-absorbing chromophore of the stratum corneum, trans-urocanic acid, using an enzyme called urocanase.
Compared to trans-urocanic acid, cis-urocanic acid is endowed with potent immunomodulatory properties. This microbial metabolism then limits the ability of cis-urocanic acid to inhibit immune responses, which means that skin bacteria fine-tune our skin’s response to UV radiation.”2
To conduct the experiment, the researchers used an animal model and closely observed how skin microbiota reacted after UVB exposure or direct application of cis-UCA. They discovered a dramatic shift wherein certain bacteria species thrived, especially those capable of metabolizing cis-UCA, such as Staphylococcus epidermidis.
• Improvements were noticed right away — One remarkable finding from the study was the speed of improvement in skin health. Within a few hours after UVB exposure, skin bacteria populations significantly shifted toward higher numbers of UCA-positive strains.
By consuming cis-UCA, the bacteria effectively lowered this compound’s concentration on the skin, preventing immunosuppression and reducing its harmful consequences like inflammation and increased susceptibility to UV-induced DNA damage. The rapid response was measurable within hours rather than days, highlighting how dynamically your skin’s microbiome responds to environmental stressors like UV radiation.
• There’s a visible improvement when beneficial bacteria thrived — Areas populated by urocanase-positive bacteria showed notably reduced signs of redness, inflammation, and other indicators of sunburn. Researchers confirmed this protective role explicitly by disinfecting the skin to remove these beneficial bacteria.
In skin lacking these microbial defenders, exposure to cis-UCA produced significantly stronger immunosuppressive effects, leading to greater inflammation and tissue damage. This stark comparison highlights the essential role these beneficial bacteria play in maintaining skin health following UV exposure.
• Not all microbes benefit from UVB exposure equally — Only bacteria with the genetic capability to produce the urocanase enzyme significantly benefited. These strains rapidly grew and dominated the skin microbiome after exposure to UVB radiation or direct cis-urocanic acid application.
• Study variables influenced skin health — The effectiveness of bacterial protection was heavily dependent on the presence of UCA-positive strains, which sharply contrasted with conditions where such bacteria were removed. This means that external interventions, such as antibacterial treatments or disinfectants commonly found in skincare products, inadvertently remove the very bacteria your skin depends on for UV protection.
• The mechanism driving the beneficial effects is straightforward — When UVB rays hit your skin, they convert the naturally occurring trans-UCA into its harmful form, cis-UCA, which actively suppresses your skin’s defenses by impairing key immune cells and reduces their ability to respond to sun-induced damage effectively.
Now, the urocanase produced by skin bacteria directly counters this threat. It transforms the cis-UCA into harmless metabolites, essentially “detoxifying” your skin surface.
Urocanase-positive bacteria drastically reduce the concentration of cis-UCA, thus helping your immune system maintain its efficiency. This reaction significantly reduces inflammation, redness, and DNA damage, which are key markers of sunburn.
• Competition as a beneficial mechanism — As urocanase-positive bacteria thrive on cis-UCA, their growth suppresses harmful microbial strains. The beneficial microbes’ success creates a healthier, more balanced microbiome on your skin, amplifying your natural defenses against environmental damage. This ecological advantage helps your skin become resilient against a range of threats, beyond just UV radiation.
• The bacterial activity creates a healthy feedback loop — When urocanase-positive bacteria thrive, their beneficial metabolites stimulate skin cells to enhance their protective barriers further, adding another layer of defense. This ongoing interaction ensures your skin not only heals quicker from sun damage but also becomes more robust against environmental stresses.
Understanding these microbial dynamics and mechanisms highlights the importance of maintaining and nurturing your skin’s microbiome for robust sun protection.
Going Deeper Into the Skin Microbiome’s Mechanisms
In a study published in Frontiers in Microbiomes, researchers examined how your skin’s microbial residents respond to UV radiation. The researchers reviewed existing evidence from multiple studies showing how your skin microbiome naturally defends against UV radiation.3
• How sunburn develops — To set the stage of the study, the researchers outlined how sunlight exposure causes sunburn that eventually damages your skin:4
“UVB interacting with keratinocytes often results in their apoptosis, leading to the formation of sunburn cells. Sun-damaged cells are characterised by their round shape, eosinophilic cytoplasm, condensed nucleus and their development leads to symptoms such as redness, pain, swelling, peeling and blisters.”
• Bacteria produce other substances that protect your skin — One key discovery outlined in the review was that several skin bacterial strains evolved their own mechanisms to resist UV damage. These microbes produce protective compounds like pigments, antioxidants, and enzymes, effectively neutralizing harmful UV radiation and minimizing its impact on your skin cells.
In one example, the bacteria Micrococcus luteus is known for its ability to withstand UV radiation by producing carotenoid pigments that resist UV rays. As a result, oxidative stress and DNA damage in your skin is reduced.
• Beneficial bacteria help manage skin conditions — The researchers noted that certain microbial strains control symptoms of certain skin conditions, such as atopic dermatitis (AD):5
“Staphylococcus cohnii is reported to modulate host anti-inflammatory pathways to protect against the development of AD. The mechanism may involve bacterially induced upregulation of the glucocorticoid production in keratinocytes, reducing the inflammation of local tissues.”
• Certain skin bacteria counteract reactive oxygen species (ROS) — UV radiation produces ROS that cause oxidative stress, damaging your skin cells and accelerating aging. Some beneficial microbes produce antioxidants or enzymes that break down these harmful molecules, effectively mitigating their damaging effects.
• The response of your skin microbiome is immediate — Microbial responses to UV exposure are rapid. Beneficial bacteria immediately begin producing protective substances after sunlight hits your skin.
Linoleic Acid — A Key Contributor to Skin Damage
An important mechanism mentioned in the Frontiers in Microbiomes study is how UVB rays interact with keratinocytes (main cells of the outermost skin layer) that lead to sunburn.
With this in mind, one important contributor is linoleic acid (LA) — an omega-6 polyunsaturated fat (PUF) largely found in vegetable oils and ultraprocessed food. While these oils are often advertised as “healthy” products because they’re made from vegetables, the reality is opposite. As noted in my 2023 study published in Nutrients, excess LA consumption leads to impaired mitochondrial function, leading to increased rates of chronic disease.6
Moreover, LA takes a long time to be purged from your system.7 But as I recently discovered, there’s a way to purge it from your skin quicker — by replacing it with a healthy fat called C15:0 (pentadecanoic acid).
• LA is embedded in your skin — The LA from your diet slowly accumulates in your tissues and cell membranes, including the keratinocytes. As your skin cells go through their cycles, the keratinocytes eventually migrate toward the surface loaded with LA.
• New skin cells form every four weeks — Research shows that keratinocytes begin their journey from the basal layer (deepest part of the epidermis) to the stratum corneum (outermost layer made of dead skin cells) around 28 days.8 Throughout this process, they form cell membranes from the fats traveling within your bloodstream by the protein albumin.9
Now, the important part that affects your health is the fat you eat. As you continue to eat a high-LA diet, your body uses this as cell membranes since it’s what’s stored in your tissues. So, even if you’ve minimized your LA intake for a few months, your keratinocytes will continue to use it since there’s still in storage.
• Lipid synthesis prefers quantity over quality — The body lacks mechanisms to eliminate LA stored in your tissues. Moreover, enzymes that play a role in phospholipid synthesis prefer abundance over quality. Again, if LA dominates your fat intake, it will be consistently used.
• C15:0 fat as the replacement — This fat is a stark contrast to LA as it contains no double bonds, making it resistant to peroxidation.10 Research shows that it’s now being recognized as an essential fat, yet most people only consume 100 to 200 milligrams of it, primarily from dairy products.11
• Add C15:0 to your diet — The great thing about C15:0 is that it acts quickly once levels rise in your body. Specifically, it’s able to integrate into the pool where lipids are derived from within weeks. From there, LA is eventually pushed out.
I’ll be posting a future article that goes over the skin cell process turnover in an in-depth manner. For now, I’ll summarize the C15:0 protocol so you can start replacing the LA embedded in your skin with healthy fats instead.
Integrate the C15:0 Protocol Into Your Routine
While the obvious route is following a low-LA diet is a wise strategy, the problem here is that it will take two to three years to fully work. But if you add 2 grams of C15:0 per day from raw, grass fed milk, the LA clearance significantly shortens to 12 to 18 months.
1. Minimize your LA intake — Take stock of your pantry and remove all vegetable oils, which include soybean, corn, sunflower, cottonseed, canola, and grapeseed oil. Aside from being used for cooking food at home, these oils are also used in restaurants and ultraprocessed food sold at grocery stores. So, be on the lookout for these products as well.
Another important point that’s seldomly discussed is the consumption of grain-fed meats. Poultry and pork products are given animal feed high in grains and LA, making them reach levels comparable to vegetable oils.
2. Take 2 grams of C15:0 per day, divided with meals — Take pure pentadecanoic acid or high-C15:0 butter or ghee concentrate. Split the dose between meals to maintain consistent plasma levels and minimize tissue uptake.
3. Track your status regularly — Take a red blood cell (RBC) test or dried-blood spot test every three months to check if your C15:0 levels are 0.4% or more and your LA is less than 5% of your total fats.
4. Support healthy fat turnover with other lifestyle changes — While C15:0 will eventually make it to your skin, I recommend incorporating high-intensity workouts, using a sauna regularly, or practicing intermittent fasting. These strategies will help remove LA faster from adipose tissue.
An important reminder about high-intensity exercise — don’t go over 75 minutes per week, otherwise it will affect your longevity and overall health. Regarding intermittent fasting, keep it short and occasionally only. That’s because long-term restrictions will depress thyroid function and metabolic rate.
5. Take it easy on sun exposure until your second summer — While you work towards removing LA from your body, understand that your skin will remain vulnerable to UV-triggered oxidative stress. During this period, avoid sunlight exposure during solar noon, especially between 11 a.m. and 3 p.m. Instead, focus on early morning or late afternoon sun exposure when the rays aren’t as intense.
Once you confirm that your LA levels are declining, your skin slowly becomes resilient. At that point, you can begin solar noon sunlight exposure without burning your skin, but do so gradually.
Lastly, avoid using conventional sunscreens, as these products block vitamin D synthesis and even hamper endocrine function. Again, slowly build your tolerance with timed, progressive exposure while supporting your health with astaxanthin, niacinamide, and vitamin E alongside healthy saturated fats from ghee, butter, and tallow.
Frequently Asked Questions (FAQs) About the Skin Microbiome
Q: What role do skin bacteria play in protecting against sun damage?
A: Certain resident skin bacteria, particularly those producing the enzyme urocanase, help protect your skin from UVB-induced damage. When your skin is exposed to UVB radiation, it converts trans-urocanic acid into cis-urocanic acid (cis-UCA), which suppresses immune responses. Urocanase-positive bacteria metabolize cis-UCA, reducing inflammation, immune suppression, and DNA damage, effectively detoxifying your skin.
Q: How does UV exposure affect the skin microbiome?
A: UVB radiation selectively promotes the growth of beneficial bacteria that metabolize cis-UCA, such as Staphylococcus epidermidis. These microbes rapidly increase in number post-exposure, providing a fast response against sun damage. Areas of the skin populated with these bacteria show less redness and inflammation, while disinfected areas lacking them suffer more severe damage, underscoring their protective role.
Q: Why should we be cautious with antibacterial skincare products and sunscreens?
A: Many conventional products disrupt skin microbiomes, wiping out beneficial bacteria that defend against UV radiation. Traditional sunscreens block UV rays but often neglect or harm these microbial allies, undermining natural immunity.
Q: What is the connection between diet, skin health, and sun resilience?
A: High intake of linoleic acid (LA), a polyunsaturated fat found in vegetable oils and grain-fed animal products, accumulates in your skin cells and increases vulnerability to sunburn. To counter this, replace LA with C15:0 (pentadecanoic acid) from sources like grass fed dairy. This switch enhances skin resilience and reduce oxidative stress over time.
Q: How can I support my skin’s natural sun defenses effectively?
A: To optimize sun protection naturally:
• Reduce LA intake by avoiding vegetable oils and grain-fed meats.
• Add 2 grams of C15:0 fat daily, split between meals.
• Track fat composition via blood tests every three months.
• Accelerate LA clearance with intermittent fasting, sauna sessions, and brief high-intensity workouts.
• Gradually build sun tolerance with early or late sunlight exposure while avoiding conventional sunscreens.
Combining these strategies supports both your skin microbiome and lipid profile, offering long-term defense against sun-related skin damage and premature aging.
- 1Journal of Investigative Dermatology, May 13, 2025
- 2News-Medical.net, May 13, 2025
- 3,4,5Front. Microbiomes 2:1102315
- 6Nutrients. 2023 Jul 13;15(14):3129
- 7Nature. 2011 Sep 25;478(7367):110–113
- 8National Cancer Institute, Layers of the Skin
- 9Science Direct, Fatty Acid Transport
- 10,11Nutrients. 2023 Oct 30;15(21):4607
Source: Original Article
Publish Date: 2025-06-10 06:00:00